‘Handover’ means different things to different disciplines and as Marcus has demonstrated is an evolved process, often specific to both medical specialty and hospital site.
To clinicians, it’s running through the Git commit history of the patients to ensure an incoming team is capable of making the mission-critical decisions over the coming shift.
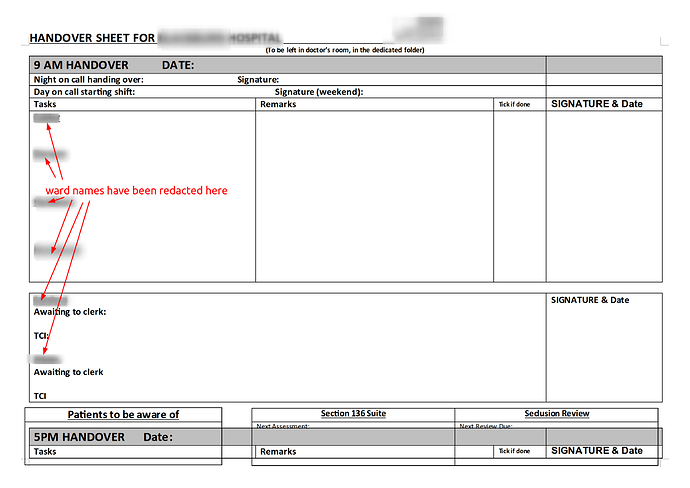
To clinical governance teams, it’s a crucial safety feature of good quality care (and as such the process should leave a patient-specific auditable footprint).
To information governance teams, it’s one of those pinch points where PID coalesces.
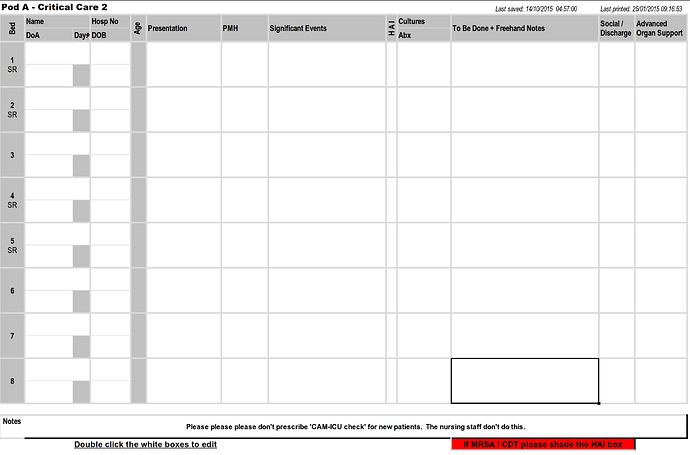
I’m an intensive care consultant, and my paper record of the handover becomes my scratchpad for ideas, prioritisation tool, aide memoire for emergency decisions (“this patient is crashing, shall we put him on the X/Y/Z?”), to do list, jotter for phone numbers and memos and a lot more besides… until it is dutifully shredded at the end of a shift when any useful information from it is either in the EPR or the brain of the incoming team.
How much of this can be distilled down into something reproducible across disparate teams and sites I would be fascinated to see, though if this were an easy challenge you’d have expected it to have been done and dusted by now.
DON’T BREAK USERLAND As you can tell from all of the above, it is a real mess at the moment, from many perspectives. But whatever solution replaces these ad-hoc arrangements MUST NOT BREAK CLINICAL WORKFLOWS. Because, bad as these handover forms may be, they are working , and we clinicians will have to continue to deliver clinical care with whatever replaces them.
Wholeheartedly agree with this. Having spent a reasonable amount of time making bad forms better (audit trail, incremental backups etc) there’s nothing more than I’d like to see than something that negates the (modest) duplication of effort, the IG concerns… but not at the expense of reducing the quality of clinical care.
Good luck, Ben!